The U.S. Food and Drug Administration today approved Tibsovo (ivosidenib) tablets for the treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) who have a specific genetic mutation. This is the first drug in its class (IDH1 inhibitors) and is approved for use with an FDA-approved companion diagnostic used to detect specific mutations in the IDH1 gene in patients with AML.
“Tibsovo is a targeted therapy that fills an unmet need for patients with relapsed or refractory AML who have an IDH1 mutation,” said Richard Pazdur, M.D., director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research. “The use of Tibsovo is associated with a complete remission in some patients and a reduction in the need for both red cell and platelet transfusions.”
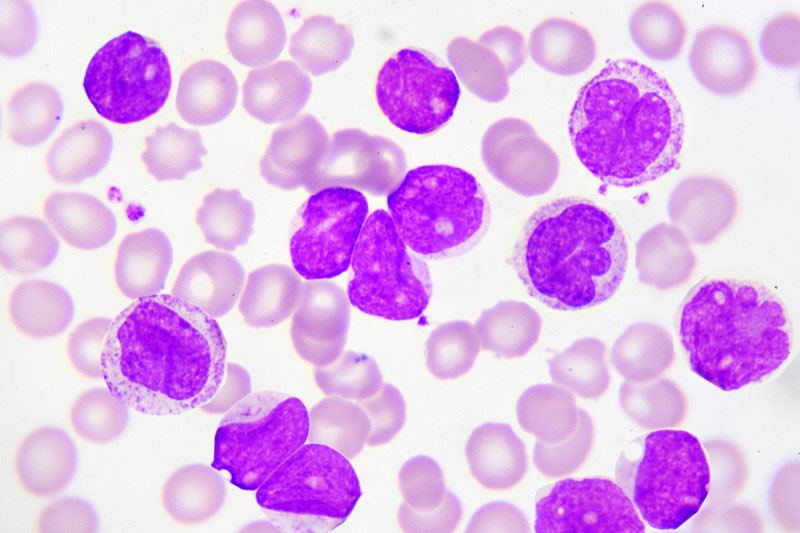
AML is a rapidly progressing cancer that forms in the bone marrow and results in an increased number of abnormal white blood cells in the bloodstream and bone marrow. The National Cancer Institute at the National Institutes of Health estimates that approximately 19,520 people will be diagnosed with AML this year; approximately 10,670 patients with AML will die of the disease in 2018.
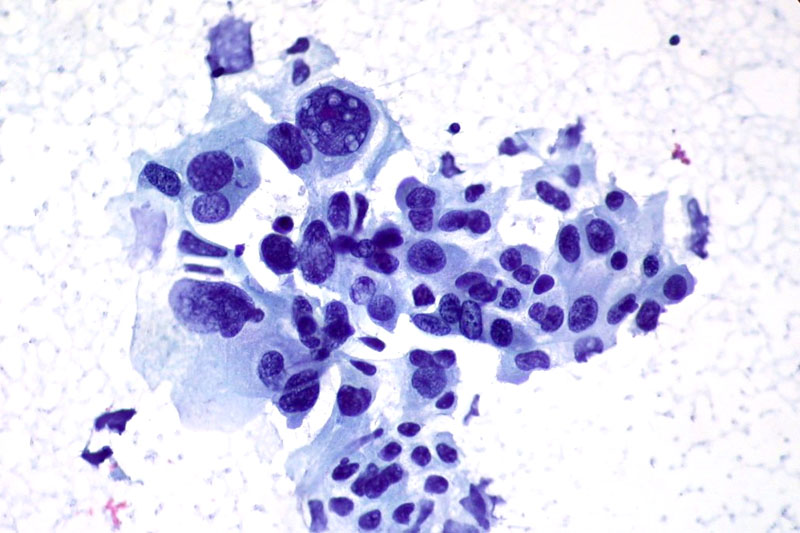
Tibsovo is an isocitrate dehydrogenase-1 inhibitor that works by decreasing abnormal production of the oncometabolite 2-hydroxyglutarate (2-HG), leading to differentiation of malignant cells. If the IDH1 mutation is detected in blood or bone marrow samples using an FDA-approved test, the patient may be eligible for treatment with Tibsovo. Today the agency also approved the RealTime IDH1 Assay, a companion diagnostic that can be used to detect this mutation.
The efficacy of Tibsovo was studied in a single-arm trial of 174 adult patients with relapsed or refractory AML with an IDH1 mutation. The trial measured the percentage of patients with no evidence of disease and full recovery of blood counts after treatment (complete remission or CR), as well as patients with no evidence of disease and partial recovery of blood counts after treatment (complete remission with partial hematologic recovery or CRh). With a median follow-up of 8.3 months, 32.8 percent of patients experienced a CR orCRh that lasted a median 8.2 months. Of the 110 patients who required transfusions of blood or platelets due to AML at the start of the study, 37 percent went at least 56 days without requiring a transfusion after treatment with Tibsovo.
Common side effects of Tibsovo include fatigue, increase in white blood cells, joint pain, diarrhea, shortness of breath, swelling in the arms or legs, nausea, pain or sores in the mouth or throat, irregular heartbeat (QT prolongation), rash, fever, cough and constipation. Women who are breastfeeding should not take Tibsovo because it may cause harm to a newborn baby.
Tibsovo must be dispensed with a patient Medication Guide that describes important information about the drug’s uses and risks. The prescribing information for Tibsovo includes a boxed warning that an adverse reaction known as differentiation syndrome can occur and can be fatal if not treated. Signs and symptoms of differentiation syndrome may include fever, difficulty breathing (dyspnea), acute respiratory distress, inflammation in the lungs (radiographic pulmonary infiltrates), fluid around the lungs or heart (pleural or pericardial effusions), rapid weight gain, swelling (peripheral edema) or liver (hepatic), kidney (renal) or multi-organ dysfunction. At first suspicion of symptoms, doctors should treat patients with corticosteroids and monitor patients closely until symptoms go away.
Other serious warnings include a QT prolongation, which can be life-threatening. Electrical activity of the heart should be tested with an electrocardiogram during treatment. Guillain-Barré syndrome, a rare neurological disorder in which the body’s immune system mistakenly attacks part of its peripheral nervous system, has happened in people treated with Tibsovo, so patients should be monitored for nervous system problems.
The FDA granted this application Fast Track and Priority Review designations. Tibsovo also received Orphan Drug designation, which provides incentives to assist and encourage the development of drugs for rare diseases.
The FDA granted the approval of Tibsovo to Agios Pharmaceuticals, Inc. The FDA granted the approval of the RealTime IDH1 Assay to Abbott Laboratories.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.