The U.S. Food and Drug Administration today approved Verzenio (abemaciclib) to treat adult patients who have hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer that has progressed after taking therapy that alters a patient’s hormones (endocrine therapy). Verzenio is approved to be given in combination with an endocrine therapy, called fulvestrant, after the cancer had grown on endocrine therapy. It is also approved to be given on its own, if patients were previously treated with endocrine therapy and chemotherapy after the cancer had spread (metastasized).
“Verzenio provides a new targeted treatment option for certain patients with breast cancer who are not responding to treatment, and unlike other drugs in the class, it can be given as a stand-alone treatment to patients who were previously treated with endocrine therapy and chemotherapy,” said Richard Pazdur, M.D., director of the FDA’s Oncology Center of Excellence and acting director of the Office of Hematology and Oncology Products in the FDA’s Center for Drug Evaluation and Research.
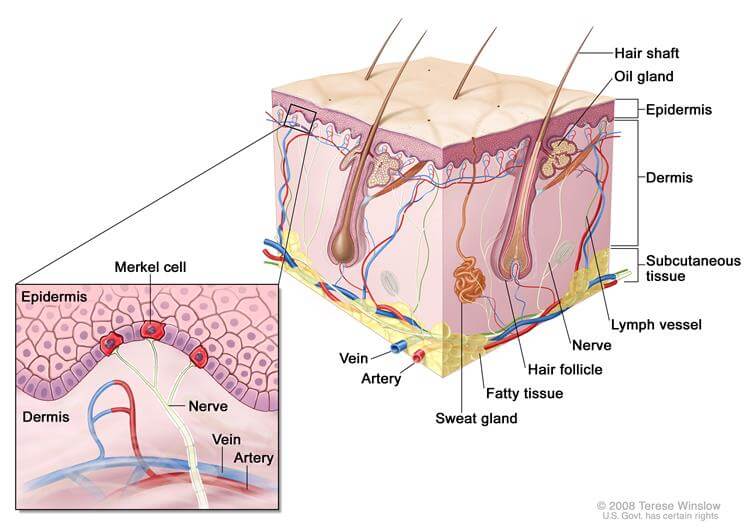
Verzenio works by blocking certain molecules (known as cyclin-dependent kinases 4 and 6), involved in promoting the growth of cancer cells. There are two other drugs in this class that are approved for certain patients with breast cancer, palbociclib approved in February 2015 and ribociclib approved in March 2017.
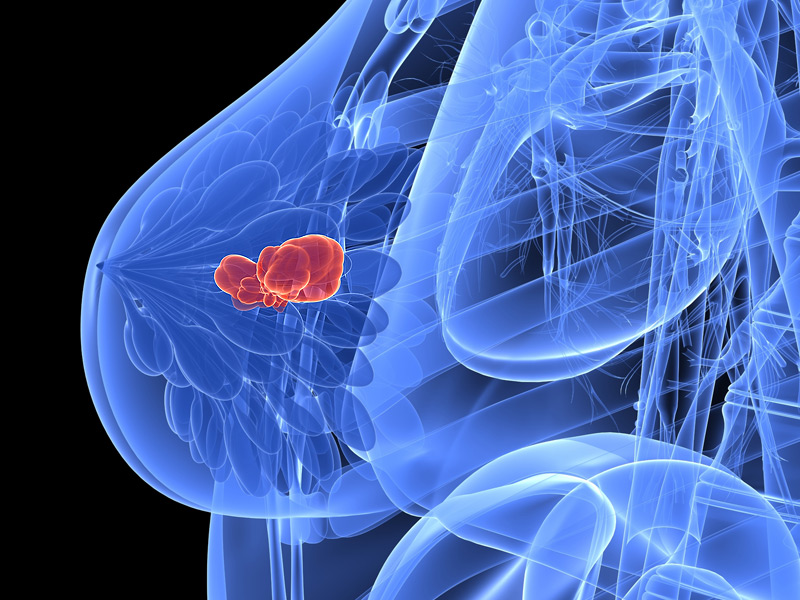
Breast cancer is the most common form of cancer in the United States. The National Cancer Institute at the National Institutes of Health estimates approximately 252,710 women will be diagnosed with breast cancer this year, and 40,610 will die of the disease. Approximately 72 percent of patients with breast cancer have tumors that are HR-positive and HER2-negative.
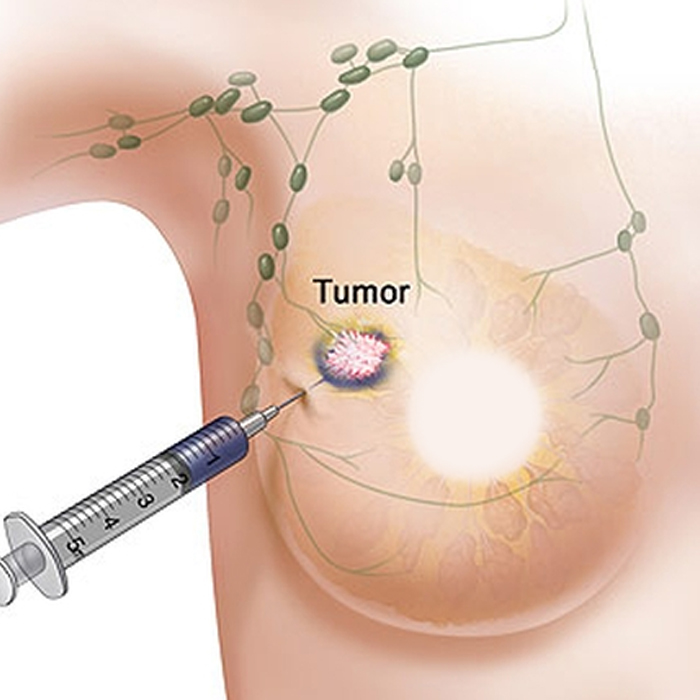
The safety and efficacy of Verzenio in combination with fulvestrant were studied in a randomized trial of 669 patients with HR-positive, HER2-negative breast cancer that had progressed after treatment with endocrine therapy and who had not received chemotherapy once the cancer had metastasized. The study measured the length of time tumors did not grow after treatment (progression-free survival). The median progression-free survival for patients taking Verzenio with fulvestrant was 16.4 months compared to 9.3 months for patients taking a placebo with fulvestrant.
The safety and efficacy of Verzenio as a stand-alone treatment were studied in a single-arm trial of 132 patients with HR-positive, HER2-negative breast cancer that had progressed after treatment with endocrine therapy and chemotherapy after the cancer metastasized. The study measured the percent of patients whose tumors completely or partially shrank after treatment (objective response rate). In the study, 19.7 percent of patients taking Verzenio experienced complete or partial shrinkage of their tumors for a median 8.6 months.
Common side effects of Verzenio include diarrhea, low levels of certain white blood cells (neutropenia and leukopenia), nausea, abdominal pain, infections, fatigue, low levels of red blood cells (anemia), decreased appetite, vomiting and headache.
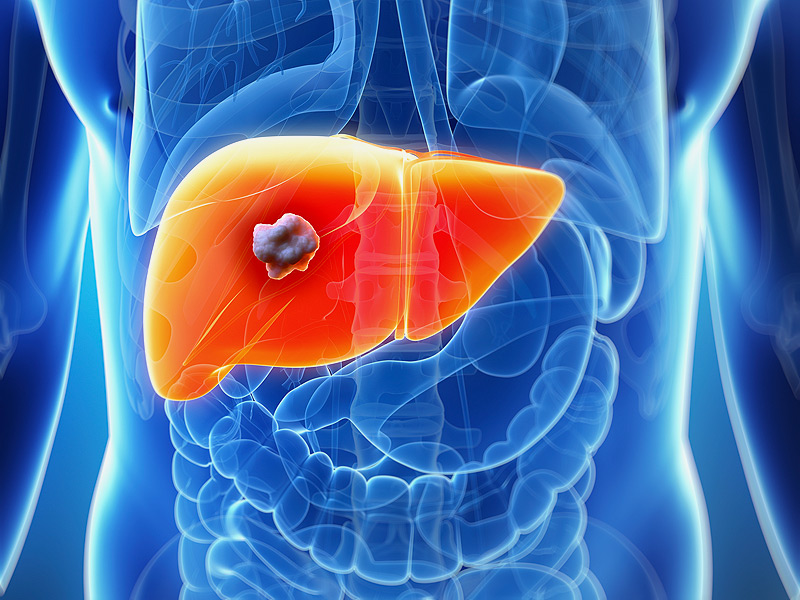
Serious side effects of Verzenio include diarrhea, neutropenia, elevated liver blood tests and blood clots (deep venous thrombosis/pulmonary embolism). Women who are pregnant should not take Verzenio because it may cause harm to a developing fetus.
The FDA granted this application Priority Review and Breakthrough Therapy designations.
The FDA granted the approval of Verzenio to Eli Lilly and Company.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.